
Improve Patient Care
Ensure patients receive all tests and treatments that are considered medical best-practice based on their demographic data – to enhance care and improve patient outcomes.
Increase Quality Scores
Close care gaps and update your EHRs to enhance your practice’s quality scores.

Maximize Funding
Access increased Medicare reimbursements based on optimal quality scores.
Without immediate access to their patients’ list of care gaps, most value-based care providers struggle to identify and address them.
Inferscience Quality Assistant lets you upload that list and integrate it directly into your EHR, so that your providers can:
Upload Patient Care Gaps
Upload your patient’s list of care gaps and let the Quality Assistant automatically analyze the information.
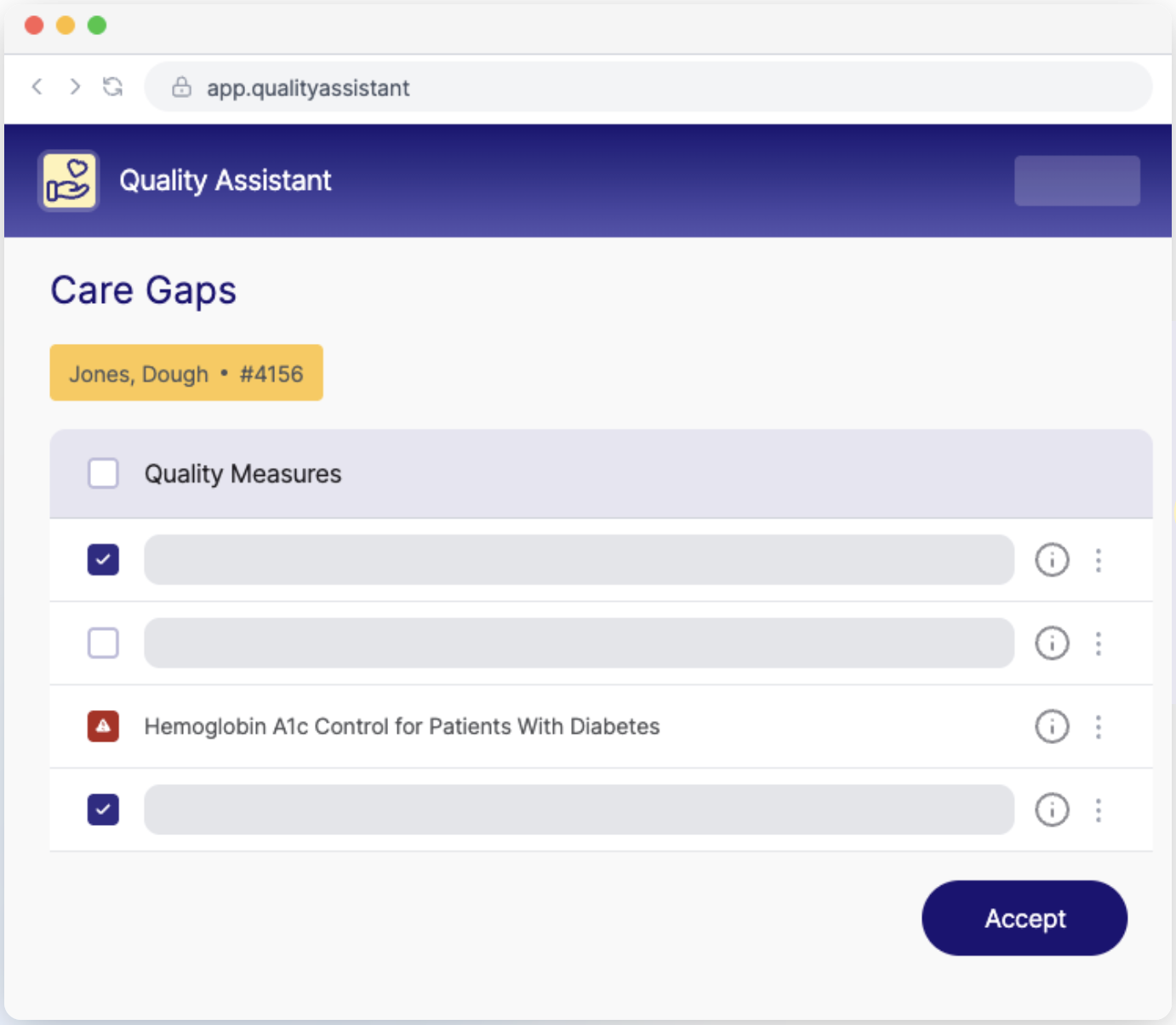
View Care Gaps
Review the suggested care gaps within your EHR and select the ones you want to document.
Close Care Gaps
Once the provider has determined which gaps are relevant, click submit to view the updated plan of care within your EHR!
There are many reasons care gaps may occur, but the most common are resource shortages and limited access to information about care gaps.
– Resource Shortages: Many healthcare practices simply lack the time or personnel required to successfully adhere to every aspect of medical “best practice”. This may lead to slow or irregular follow-ups, missed scans or checks, or a slow intervention which misses opportunities to “catch” an illness in its early stages.
– Limited Information: Care gaps can also be caused by a lack of access to data or insight. Many practices keep a record of all care gaps, but these are often not read to hand when physicians are seeing patients. As a result, the physician is not reminded of the gap – and the care gap is not closed.
There are many examples of care gaps, such as:
– Gaps in Diabetes Care: A patient with diabetes has not had an HbA1c test performed in the last 12 months, despite guidelines recommending this test at least twice a year for patients meeting treatment goals and quarterly for those not meeting goals.
– Gaps in Mental Health Care: A patient hospitalized for severe depression is discharged with a treatment plan that includes weekly therapy sessions and medication management. However, they do not receive a scheduled follow-up appointment or adequate support to manage their medication regimen.
– Gaps in Nursing Care: A patient recovering from surgery reports moderate to severe pain during routine nursing rounds. But the nurse does not document the patient’s pain or fails to use a standardized pain assessment tool.
– Gaps in Primary Care: A 45-year-old patient visits their primary care provider (PCP) for an annual wellness check. Despite risk factors such as obesity and a family history of diabetes, the PCP does not screen for early signs of hypertension or prediabetes.