Bridging the gap between payers and providers
with real-time insights.


Our solutions use advanced natural language processing (NLP) and clinical logic to bring together structured and unstructured patient data from the EHR, health information exchanges (HIEs), and claims. This enables your organization to:
Our products work together to transform complex clinical data into actionable insights, reducing administrative burden while improving quality performance and documentation accuracy across your organization.
Our NLP analyzes structured notes, unstructured text, and historical data to surface clinically supported HCC codes in real time.
Identify chronic conditions, recapture opportunities, and overlooked diagnoses to strengthen RAF accuracy and boost Medicare Advantage reimbursement.
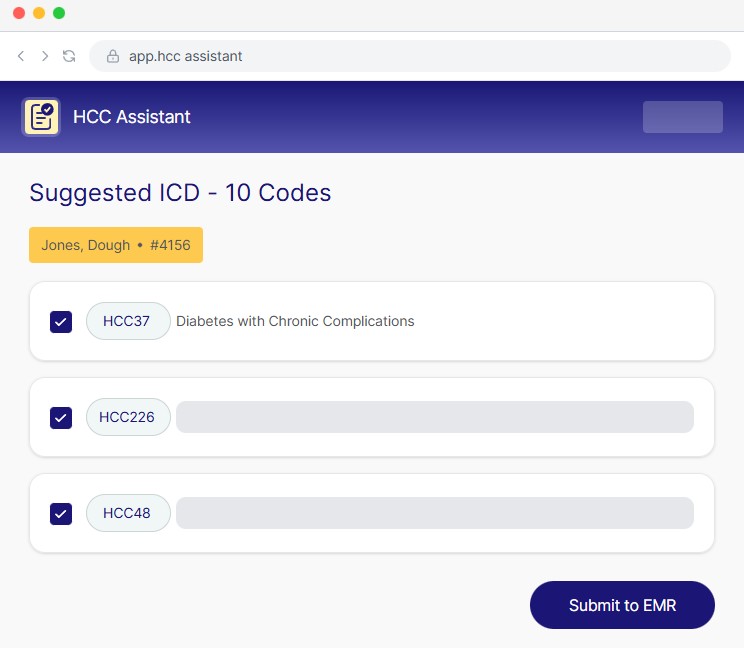
Flags existing and potential HCC conditions directly in the EHR for faster, more accurate decision-making at the point of care.
Provides a digital trail showing exactly why a code is suggested, strengthening compliance and audit readiness.
Surface needed labs, screenings, and other gaps so providers can act during the visit.
Reduce missed gaps by surfacing payer requirements inside the EHR for point-of-care action.
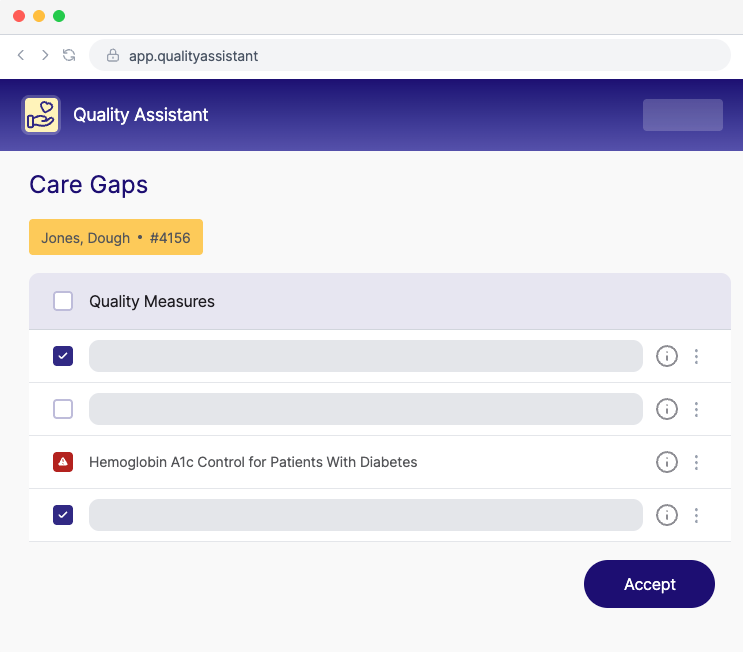
Close more gaps accurately and on time to strengthen value-based performance.
Eliminate portal logins & manual reconciliation by bringing care gap data into the EHR.
Bring diagnoses, meds, labs, imaging, notes and more into one clear, synthesized snapshot so clinicians don’t have to spend extra time clicking through the EHR.
Ask patient-specific questions and receive instant, evidence-informed answers sourced directly from chart data and external documents.
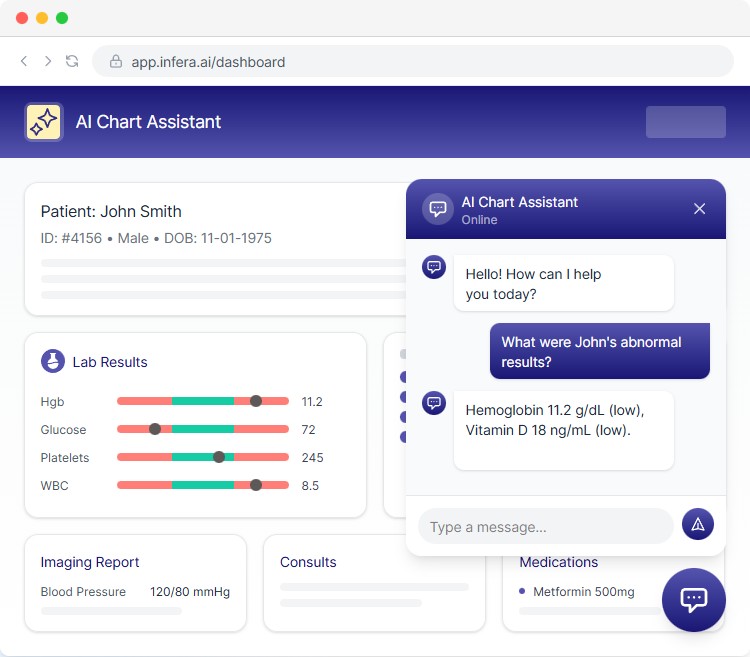
Automatically ingest and interpret referrals, hospital reports, and scanned PDFs to ensure the full picture is always available.
Get a fast, AI-powered overview of what’s clinically relevant for the upcoming visit, reducing prep time and cognitive load.
Ensure every diagnosis is fully documented before submission, reducing audit risk and strengthening RAF accuracy.
Automatically flags ICD-10 codes most likely to trigger scrutiny so plans can correct issues before they become liabilities.
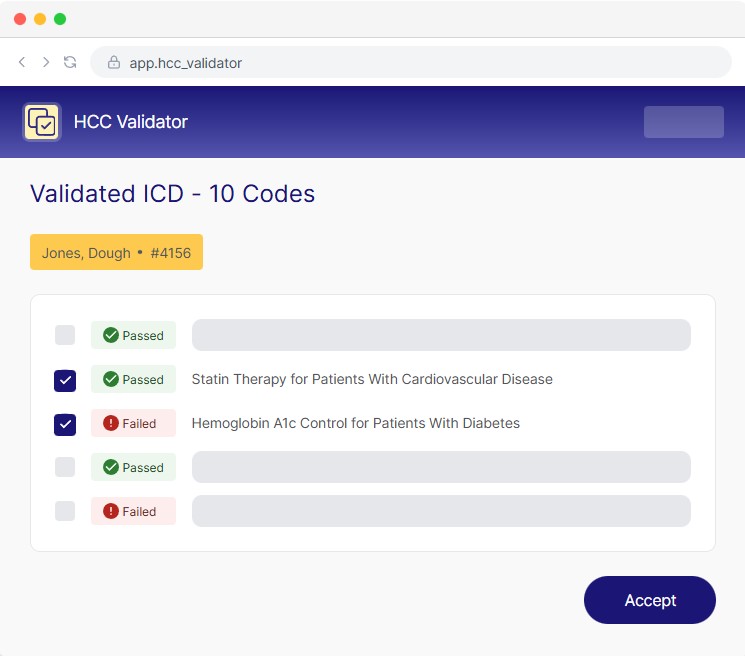
Delivers instant, actionable recommendations during documentation to help clinicians submit defensible, compliant diagnoses
Generates clear, structured evidence trails that simplify RADV preparation and protect plans from costly recoupments.
Inferscience AI solutions integrate seamlessly with your EHR for maximum efficiency






“In 8 months, our organization has presented more than 269K HCC codes to Providers and Advance Providers. Our coders and 300+ primary care providers find it to be very straightforward and user friendly.”
athenaOne User
Billing Staff, Multispecialty
athenaOne User
Administrative Staff, Multispecialty
“It has been a great opportunity to work with the Inferscience program, it is very user friendly. It enhances our accuracy and consistency with the HCC coding and allows us to produce quality service for our providers.”
athenaOne User
Administrative/Clerical Staff, Multispecialty

We have a lot to say! Here is a collection of valuable information on HCC Risk Adjustment Coding, Clinical Decisions Support, healthcare quality, the business of healthcare and clinical issues as well as Inferscience news.